Healthy Weight
Learn what it takes to get to a healthy weight (and stay there!).
You may not get down to the number you saw on the scale 20 years ago, but you can still get to a weight that enhances your health and your life.
First, what does “healthy weight” mean to you? Is it the weight you think you should be? The same as you weighed 20 years ago? Ten pounds less than your sister-in-law? We can’t provide an exact number for you personally, but we can give you some pointers on how to get to a weight that’s healthy for you and stay there.
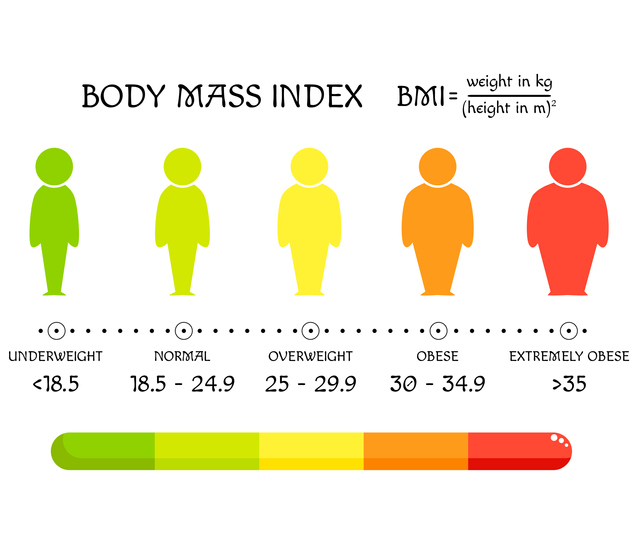
Two ways to get a ballpark idea if your weight is healthy or not: body mass index (BMI) and waist circumference.
BMI measures your height compared to your weight. For example, a person who is 5’7” and weighs 170 pounds has a BMI of 26.6, which is in the overweight range:
But experts note that BMI doesn’t measure belly fat, and that’s important. Too much belly fat can increase your risk for type 2 diabetes, heart disease, and stroke. Waist circumference (waist size) takes belly fat into account and helps predict your risk of health problems from being overweight. Women whose waist measures more than 35 inches and men whose waist measures more than 40 inches are at higher risk. Losing weight can reduce belly fat and lower that risk!
To measure your waist correctly, stand and place a tape measure around your middle, just above your hipbones. Measure your waist just after you breathe out.
Read about these three people who were able to shed the pounds (and keep them off).
Getting Started
Losing weight doesn’t have to mean losing a lot of weight. Taking off just 5% to 10%—that’s 10 to 20 pounds for a 200-pound person—can improve your health and well-being. If you have diabetes, you may find your blood sugar levels are easier to manage and that you need less diabetes medicine after you lose weight. Many people who lose weight notice that they have more energy and sleep better too.
A healthy weight goal is one thing; dropping the pounds is quite another. If there were an easy way to lose weight and keep it off, everyone would be doing it. We’ve all known someone who follows a popular diet plan and loses weight fast but then gains it all back (and then some). After trying and failing over and over, it’s easy to see why people give up.
Food for Life
Instead, create an eating plan that you can follow for life. It just needs two key ingredients:
- It’s based on healthy food.
- You can keep doing it long term.
With that in mind, you may need to try different things to figure out what works best for you day to day. Some people cut back on sugar and eat more protein to stay fuller longer. Others focus on filling up with extra fruits and vegetables, which leaves less room for unhealthy food. Still others limit variety for most meals and stick with choices that they know are healthy and filling. The details will depend on what you like and what fits in best with your life. If you need ideas and support, talk to a registered dietitian or diabetes educator (your doctor can give you a referral).
Physical Activity
Physical activity can make you feel better, function better, and sleep better. You’re not likely to lose a lot of weight with physical activity alone, but combining it with your diet strategy can improve weight loss. Here are the basic guidelines:
- Every week: do at least 150 minutes of moderate physical activity, such as brisk walking, or 75 minutes of vigorous activity, such as jogging, or an equivalent combination of the two.
- Two or more days a week: do strength-training activities, such as lifting weights or using a resistance band, that involve all major muscle groups.
If you have diabetes, physical activity can help you manage the condition along with your weight. Being active makes you more sensitive to insulin (the hormone that allows cells in your body to use blood sugar for energy). Your body won’t need to make as much insulin or you won’t need to take as much. Lower insulin levels can help prevent fat storage and weight gain. Learn more about being active when you have diabetes here.
While how you lose weight will be highly personalized, these pointers have helped others reach their goal and could help you, too.
Willpower Isn’t Enough
Don’t get us wrong: willpower is great. It just isn’t enough. You can’t count on it to reach and maintain the healthier weight you want.
But don’t worry; there are other ways. Control your environment so temptation is out of the picture and healthy habits are in. Some ideas:
- Don’t bring home food you don’t want to eat. Make home a safe zone!
- Avoid buffet-style restaurants.
- Don’t let yourself get too hungry.
- Cook your own food so you can control the calories.
- Lay out your workout clothes before you go to sleep.
- Keep the dog’s leash and your walking shoes by the door.
Sleep Helps
Too little sleep makes dieting much harder because it increases your hunger and appetite, especially for high-calorie, high-carb foods. Too little sleep also triggers stress hormones, which tell your body to hang onto fat. Outsmart this problem by being physically active, which has been shown to help you fall asleep faster and sleep better. A relaxing nighttime routine can also help you get your zzz’s. And these tips are tried and true: no screens an hour before bedtime, avoid heavy meals and alcohol before bedtime, and keep your bedroom dark and cool.
Balancing Food and Activity
Try this interactive Body Weight Planner to calculate calories and activity needed to get to your goal weight and maintain it.
Write It When You Bite It
Writing down what you eat is the single best predictor of weight loss success. But most people don’t do it because they think it will be too time-consuming. Guess how long it takes (yes, studies have been done)? Less than 15 minutes a day on average. You don’t need to add lots of detail, but aim for at least 3 entries each day and do it consistently day after day for the best results. Use this handy food diary [PDF – 105 KB] to get started.
Find Your Motivation
People who keep the weight off tend to be motivated by more than just being thinner. For some, it might be a health scare. Others want more energy to play with their grandkids. Focus on a goal that’s meaningful to you, and you’ll be more likely to keep the pounds off too.
More Tips
- Eat higher-protein, lower-carb meals to control hunger and appetite. For people with diabetes who take insulin, eating fewer carbs like bread, pasta, rice, desserts, sugary beverages, and juice can lower how much insulin they need. Using less insulin can help prevent hunger, fat storage, and weight gain.
- Choose carbs that are higher in fiber and lower in added sugar. For example, say yes to beans and sweet potatoes; say no to sugary drinks and chips.
- Drink more water and fewer sweetened beverages. This one change can cut lots of calories and mean fewer blood sugar swings!
- Keep moving. Physical activity helps you stay motivated and keep the weight off.
- Learn from a bad day. Everyone slips up from time to time; figure out what went wrong and plan for it next time. You’re only human, and humans are great learners.