Chest Cold (Acute Bronchitis)
Cough keeping you up at night? Soreness in your chest and feeling tired? You could have a chest cold.
Antibiotics will not help you get better if you have a chest cold (acute bronchitis).
If you’re healthy without heart or lung problems or a weakened immune system, this information is for you.
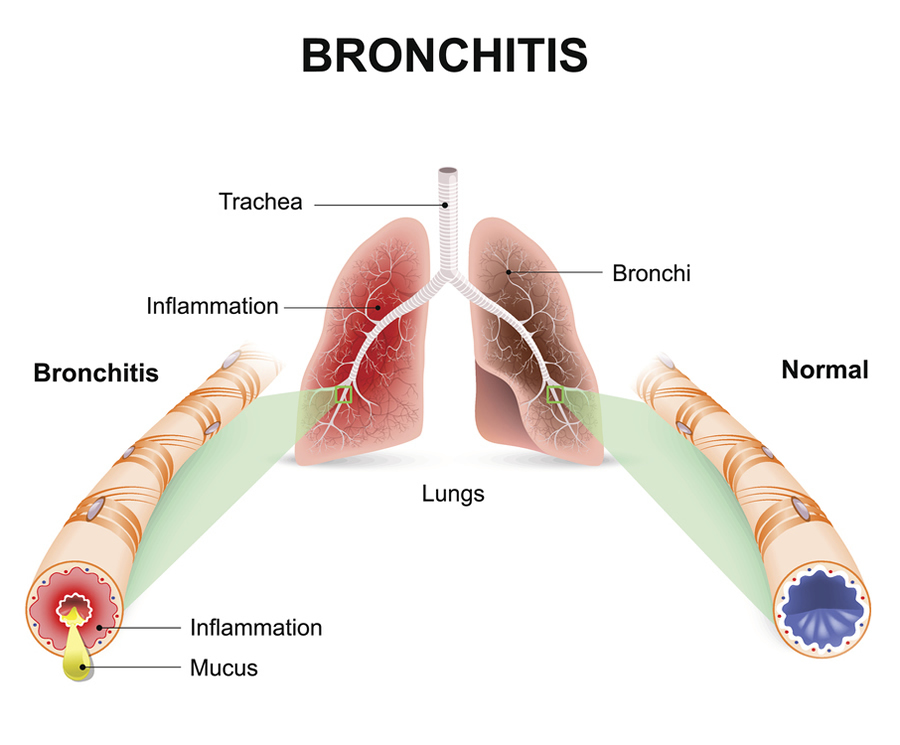
What is a chest cold (acute bronchitis)?
A chest cold, often called acute bronchitis, occurs when the airways of the lungs swell and produce mucus in the lungs. That’s what makes you cough. Acute bronchitis can last less than 3 weeks.
Causes
A virus usually causes acute bronchitis. Bacteria can sometimes cause acute bronchitis. But, even in these cases, taking antibiotics is NOT advised and will not help you get better.
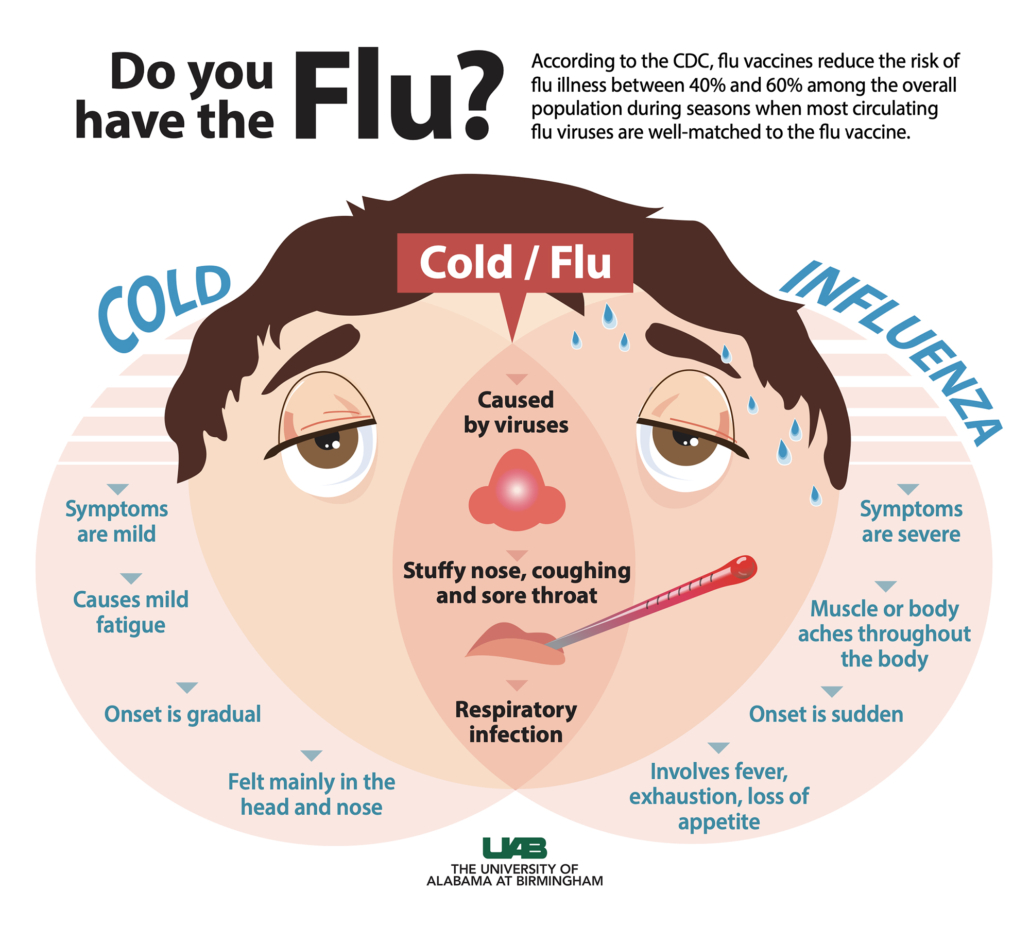
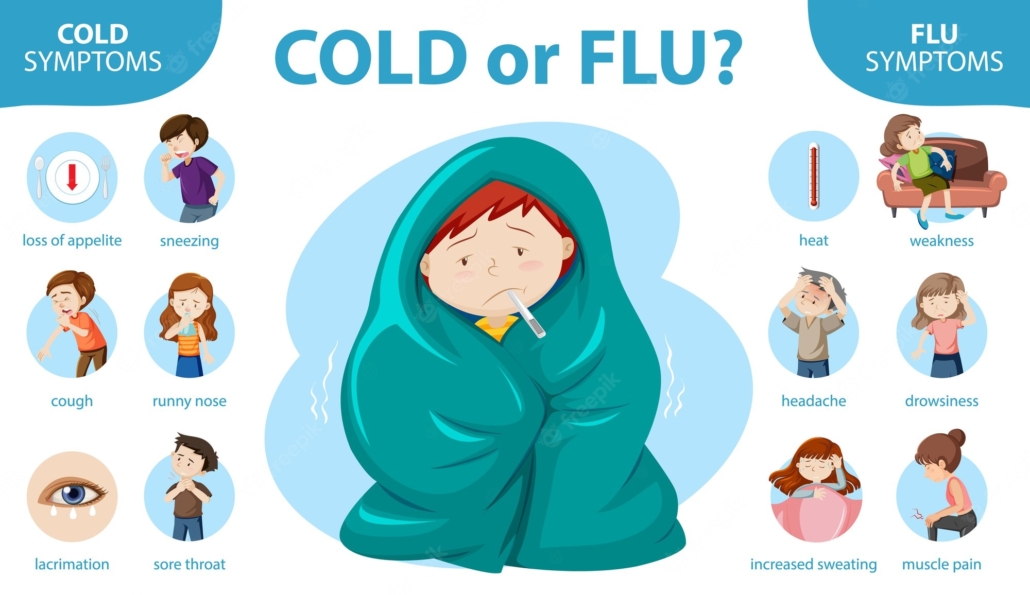
Symptoms
Symptoms of acute bronchitis last less than 3 weeks and can include:
- Coughing with or without mucus
- Soreness in the chest
- Feeling tired (fatigue)
- Mild headache
- Mild body aches
- Sore throat
When to Seek Medical Care
Talk to a healthcare professional right away if your child is under 3 months old with a fever of 100.4 °F (38 °C) or higher.
See a doctor if you have any of the following:
- Temperature of 100.4 °F or higher
- Cough with bloody mucus
- Shortness of breath or trouble breathing
- Symptoms that last more than 3 weeks
- Repeated episodes of bronchitis
This list is not all-inclusive. Please see a doctor for any symptom that is severe or concerning.
Treatment
Acute bronchitis usually gets better on its own—without antibiotics. Antibiotics won’t help you get better if you have acute bronchitis.
When antibiotics aren’t needed, they won’t help you, and their side effects could still cause harm. Side effects can range from mild reactions, like a rash, to more serious health problems. These problems can include severe allergic reactions, antibiotic-resistant infections and C. diff infection. C. diff causes diarrhea that can lead to severe colon damage and death.
Other illnesses like whooping cough (pertussis) or pneumonia can have similar symptoms to acute bronchitis. If you have whooping cough or pneumonia, your doctor will most likely prescribe antibiotics.
How to Feel Better
Below are some ways you can feel better while your body fights off acute bronchitis:
- Get plenty of rest.
- Drink plenty of fluids.
- Use a clean humidifier or cool mist vaporizer.
- Use saline nasal spray or drops to relieve a stuffy nose.
- For young children, use a rubber suction bulb to clear mucus.
- Breathe in steam from a bowl of hot water or shower.
- Suck on lozenges. Do not give lozenges to children younger than 4 years of age.
- Use honey to relieve cough for adults and children at least 1 year of age or older.
Ask your doctor or pharmacist about over-the-counter medicines that can help you feel better. Always use over-the-counter medicines as directed. Remember, over-the-counter medicines may provide temporary relief of symptoms, but they will not cure your illness.
Over-the-Counter Medicine and Children
Carefully read and follow instructions on over-the-counter medicine product labels before giving medicines to children. Some over-the-counter medicines are not recommended for children of certain ages.
- Pain relievers:
- Children younger than 6 months: only give acetaminophen.
- Children 6 months or older: it is OK to give acetaminophen or ibuprofen.
- Never give aspirin to children because it can cause Reye’s syndrome. Reye’s syndrome is a very serious, but rare illness that can harm the liver and brain.
- Cough and cold medicines:
- Children younger than 4 years old: do not use over-the-counter cough and cold medicines in young children unless a doctor specifically tells you to. Cough and cold medicines can result in serious and sometimes life-threatening side effects in young children.
- Children 4 years or older: discuss with your child’s doctor if over-the-counter cough and cold medicines are safe to give to your child.
Ask your doctor or pharmacist about the right dosage of over-the-counter medicines for your child’s age and size. Also, tell your child’s doctor and pharmacist about all prescription and over-the-counter medicines they are taking.
Prevention
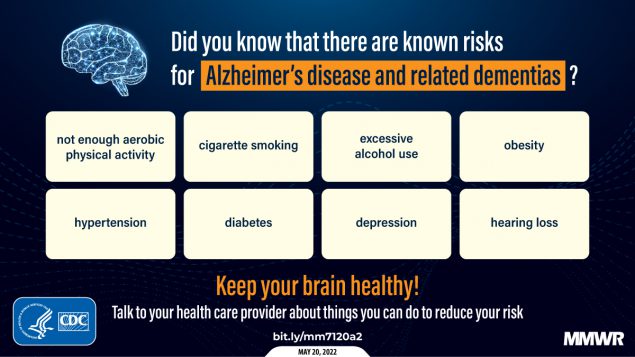
You can help prevent acute bronchitis by doing your best to stay healthy and keep others healthy, including:
- Clean your hands.
- Get recommended vaccines, such as the flu vaccine.
- Don’t smoke and avoid secondhand smoke.
- Cover your mouth and nose when coughing or sneezing.