Top 10 Most Common Health Issues
- Physical Activity and Nutrition
- Overweight and Obesity
- Tobacco
- Substance Abuse
- HIV/AIDS
- Mental Health
- Injury and Violence
- Environmental Quality
- Immunization
- Access to Health Care
Physical Activity and Nutrition
Research indicates that staying physically active can help prevent or delay certain diseases, including some cancers, heart disease and diabetes, and also relieve depression and improve mood. Inactivity often accompanies advancing age, but it doesn’t have to. Check with your local churches or synagogues, senior centers, and shopping malls for exercise and walking programs. Like exercise, your eating habits are often not good if you live and eat alone. It’s important for successful aging to eat foods rich in nutrients and avoid the empty calories in candy and sweets.
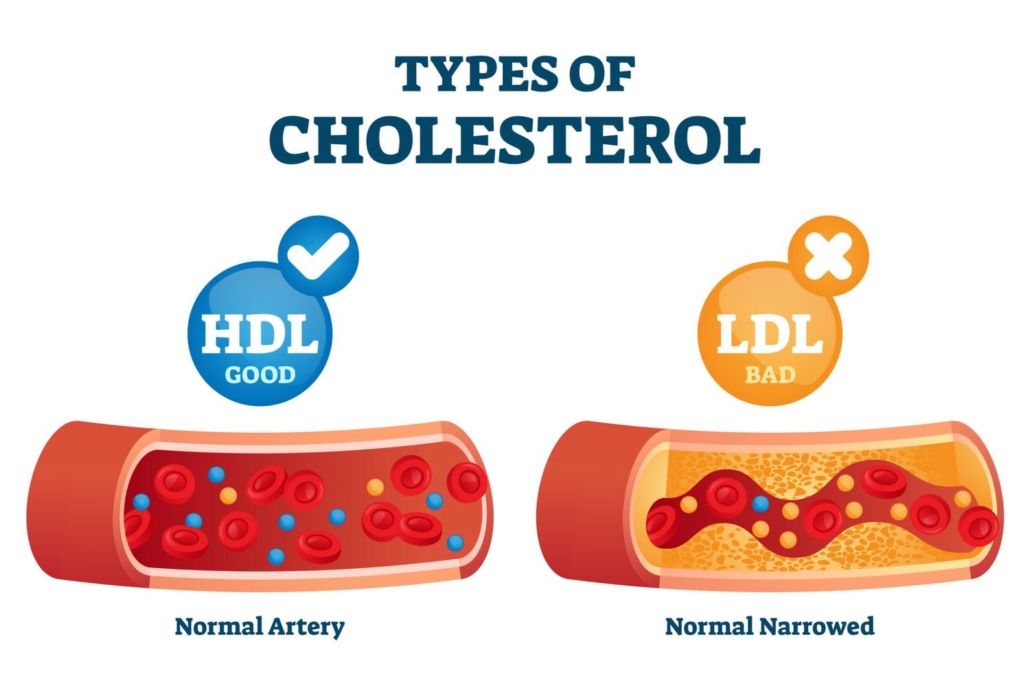
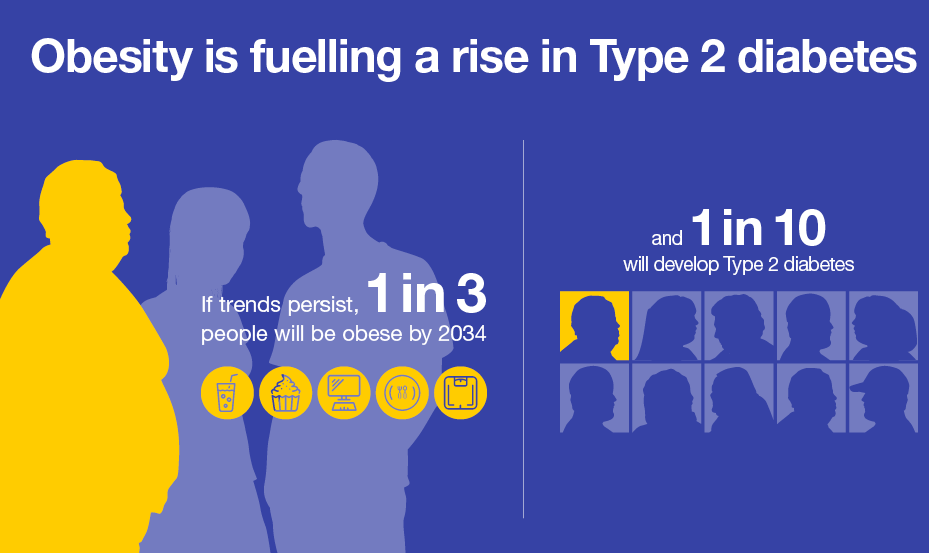
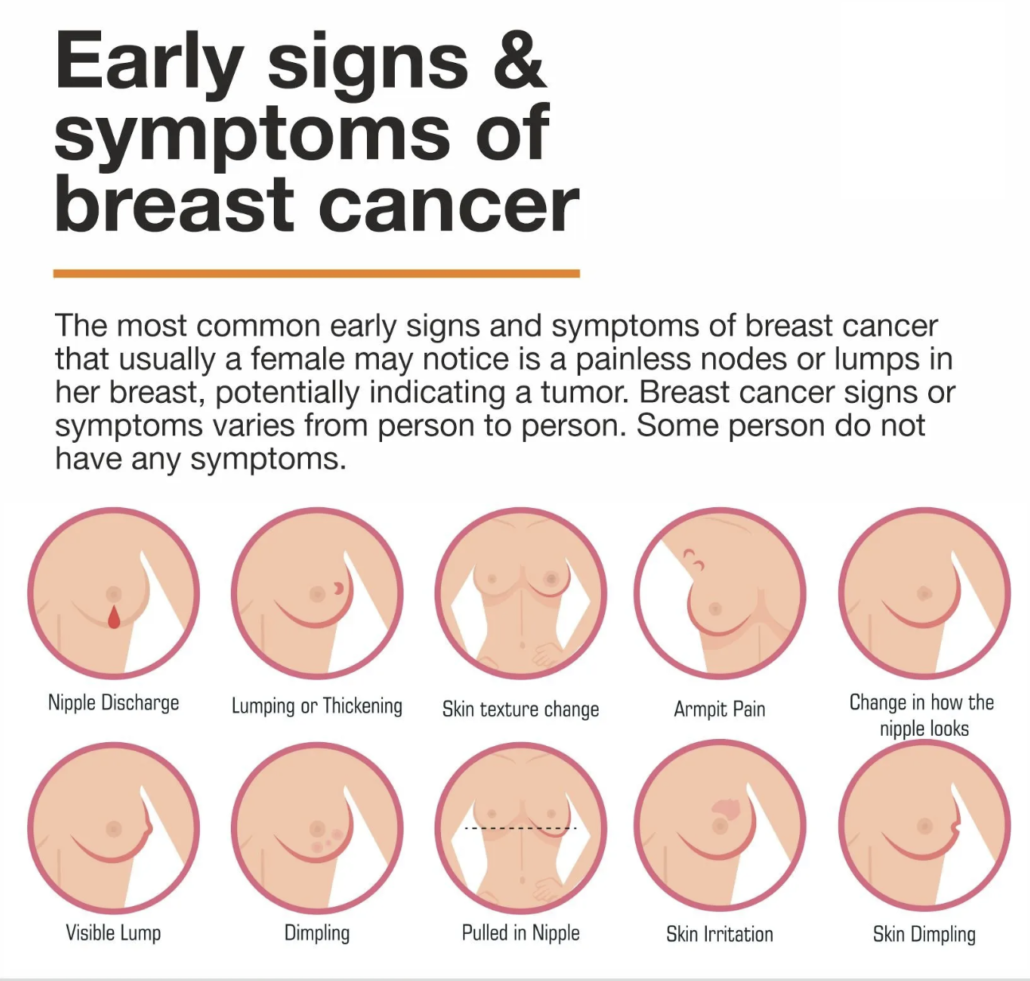
Overweight and Obesity
Being overweight or obese increases your chances of dying from hypertension, type 2 diabetes, coronary heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnea, respiratory problems, dyslipidemia and endometrial, breast, prostate, and colon cancers. In-depth guides and practical advice about obesity are available from the National Heart Lung and Blood Institute of the National Institutes of Health.
Tobacco
Tobacco is the single greatest preventable cause of illness and premature death in the U.S. Tobacco use is now called “Tobacco dependence disease.” The Centers for Disease Control and Prevention (CDC) says that smokers who try to quit are more successful when they have the support of their physician.
Substance Abuse
Substance abuse usually means drugs and alcohol. These are two areas we don’t often associate with seniors, but seniors, like young people, may self-medicate using legal and illegal drugs and alcohol, which can lead to serious health consequences. In addition, seniors may deliberately or unknowingly mix medications and use alcohol. Because of our stereotypes about senior citizens, many medical people fail to ask seniors about possible substance abuse.
HIV/AIDS
Between 11 and 15% of U.S. AIDS cases occur in seniors over age 50. Between 1991 and 1996, AIDS in adults over 50 rose more than twice as fast as in younger adults. Seniors are unlikely to use condoms, have immune systems that naturally weaken with age, and HIV symptoms (fatigue, weight loss, dementia, skin rashes, swollen lymph nodes) are similar to symptoms that can accompany old age. Again, stereotypes about aging in terms of sexual activity and drug use keep this problem largely unrecognized. That’s why seniors are not well represented in research, clinical drug trials, prevention programs and efforts at intervention.
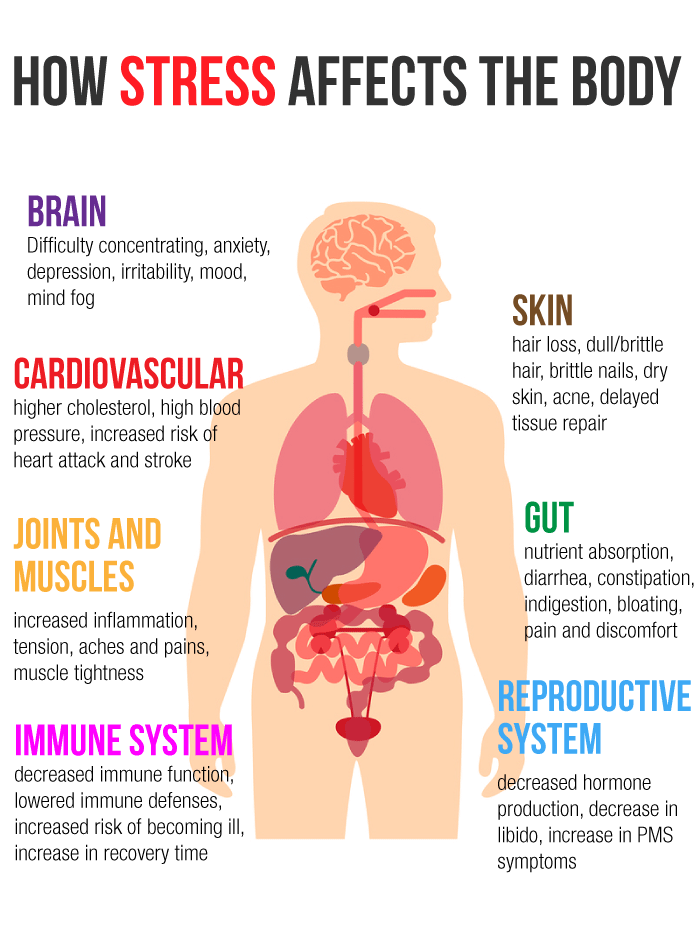
Mental Health
Dementia is not part of aging. Dementia can be caused by disease, reactions to medications, vision and hearing problems, infections, nutritional imbalances, diabetes, and renal failure. There are many forms of dementia (including Alzheimer’s Disease) and some can be temporary. With accurate diagnosis comes management and help. The most common late-in-life mental health condition is depression. If left untreated, depression in the elderly can lead to suicide. Here’s a surprising fact: The rate of suicide is higher for elderly white men than for any other age group, including adolescents.
Injury and Violence
Among seniors, falls are the leading cause of injuries, hospital admissions for trauma, and deaths due to injury. One in every three seniors (age 65 and older) will fall each year. Strategies to reduce injury include exercises to improve balance and strength and medication review. Home modifications can help reduce injury. Home security is needed to prevent intrusion. Home-based fire prevention devices should be in place and easy to use. People aged 65 and older are twice as likely to die in a home fire as the general population.
Environmental Quality
Even though pollution affects all of us, government studies have indicated that low-income, racial and ethnic minorities are more likely to live in areas where they face environmental risks. Compared to the general population, a higher proportion of elderly are living just over the poverty threshold.
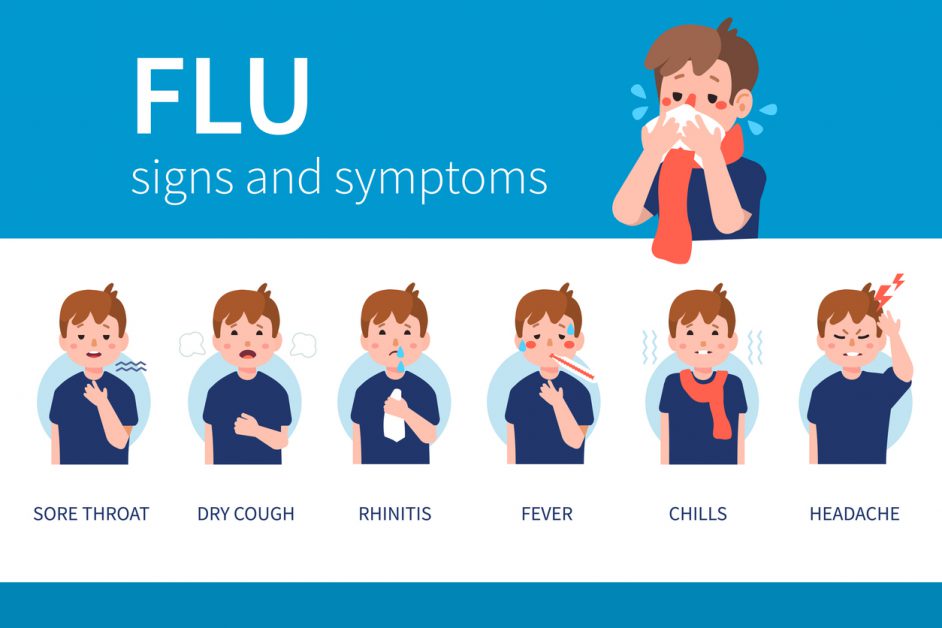
Immunization
Influenza and pneumonia and are among the top 10 causes of death for older adults. Emphasis on Influenza vaccination for seniors has helped. Pneumonia remains one of the most serious infections, especially among women and the very old.
Access to Health Care
Seniors frequently don’t monitor their health as seriously as they should. While a shortage of geriatricians has been noted nationwide, URMC has one of the largest groups of geriatricians and geriatric specialists of any medical community in the country. Your access to health care is as close as URMC, offering a menu of services at several hospital settings, including the VA Hospital in Canandaigua, in senior housing, and in your community.