What to know about sleep deprivation
Many people do not get enough quality sleep, and this can affect their health, well-being, and ability to do everyday activities.
The right amount of sleep can vary from person to person, but the Centers for Disease Control and Prevention (CDC) recommend that adults get at least 7 hours each night. They also estimate that 1 in 3 adults do not get enough sleep.
Occasional interruptions to sleep can be a nuisance, while an ongoing lack of quality sleep can affect a person’s performance at work or school, their ability to function day to day, their quality of life, and their health.
This article looks at the effects of sleep deprivation and how to treat and prevent it.
How much sleep do people need?
The CDC recommend the following amounts of sleep in every 24-hour period:
| Age | Hours of sleep |
| 4–12 months | 12–16, including naps |
| 1–2 years | 11–14, including naps |
| 3–5 years | 10–13, including naps |
| 6–12 years | 9–12 |
| 13–18 years | 8–10 |
| 18–60 years | 7 or more |
It is important to consider quality, as well as quantity, of sleep. If a person has low-quality sleep, they feel tired the next day, regardless of how many hours they have slept.
Low-quality sleep may involve:
- waking often during the night
- breathing difficulties, such as sleep apnea
- an environment that is too hot, cold, or noisy
- an uncomfortable bed
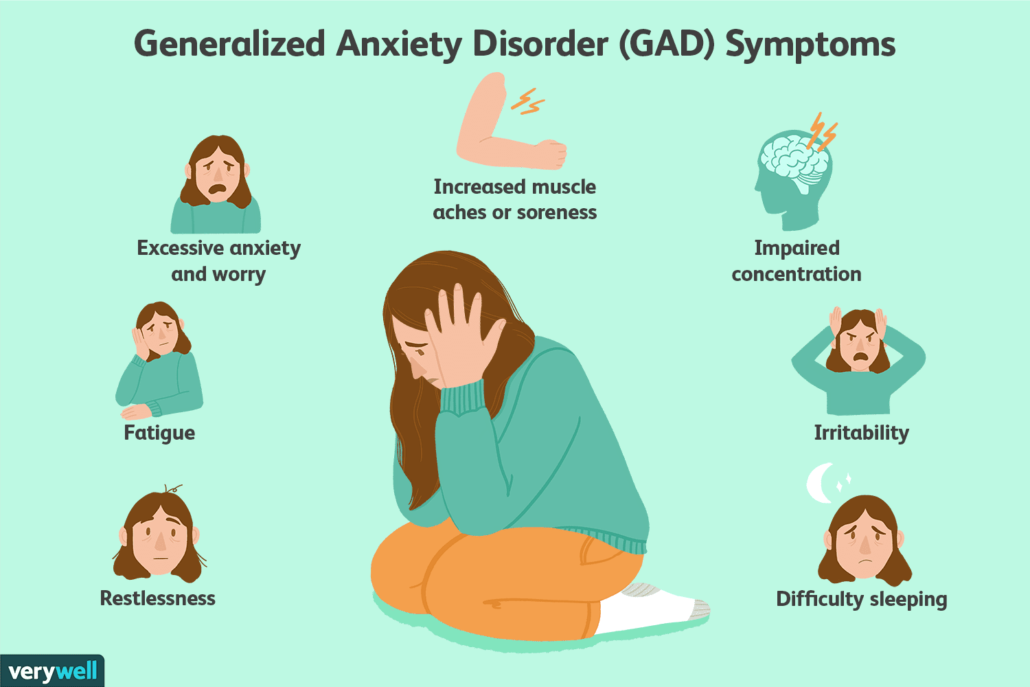
Symptoms of sleep deprivation
A person who is getting too little quality sleep may experience a range of symptoms, including:
- fatigue
- irritability
- mood changes
- difficulty focusing and remembering
- a reduced sex drive
Effects on the body
Sleep deprivation can affect various aspects of health, including:
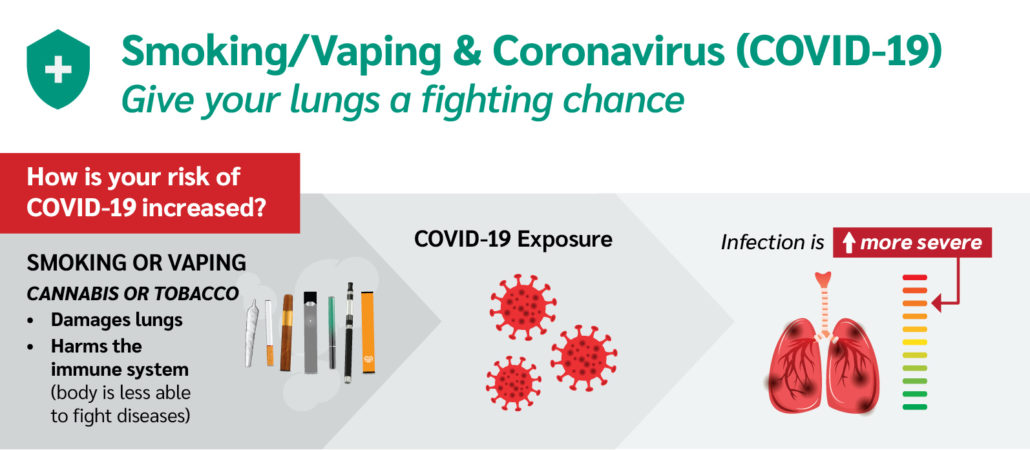
- The immune system: Sleep deprivation may cause a person to be more prone to infections, which may take longer to resolve, and respiratory diseases.
- Weight: Sleep can affect the hormones that control feelings of hunger and fullness. It can also trigger the release of insulin. Changes to sleep can cause increased fat storage, changes in body weight, and a higher risk of type 2 diabetes.
- The cardiovascular system: Sleep helps the heart vessels heal and rebuild and affects processes that maintain blood pressure, sugar levels, and inflammation control. Too little sleep may increase the risk of cardiovascular disease.
- Hormone levels: Insufficient sleep can affect hormone production, including the production of growth hormones and testosterone. It also causes the body to release additional stress hormones, such as norepinephrine and cortisol.
- The brain: Sleep deprivation affects the prefrontal cortex, which handles reasoning, and the amygdala, which deals with emotion. A lack of sleep may also make it harder for a person to form new memories, which can affect learning.
- Fertility: Poor sleep may affect the production of hormones that boost fertility.
Increased risk of accidents
A lack of sleep can limit the ability to:
- pay attention
- react quickly
- make decisions
A person who gets too little sleep may have a higher risk of drowsy driving, which can lead to accidents. In one survey, 1 in 25 adults in the U.S. said that they had fallen asleep at the wheel within the last month.
People should not drive or use machinery if they feel drowsy.
Long-term effects and complications
In the long term, having too little sleep may increase the risk of:
- hypertension
- diabetes or insulin resistance
- sleep apnea
- obesity
- heart attack
- stroke
- depression and anxiety
- psychosis
Causes
There are many reasons why a person may not get enough sleep. Examples include:
- shift work
- meeting deadlines
- a sleeping environment that is noisy or not the right temperature
- using electronic devices close to bedtime or keeping them in the bedroom
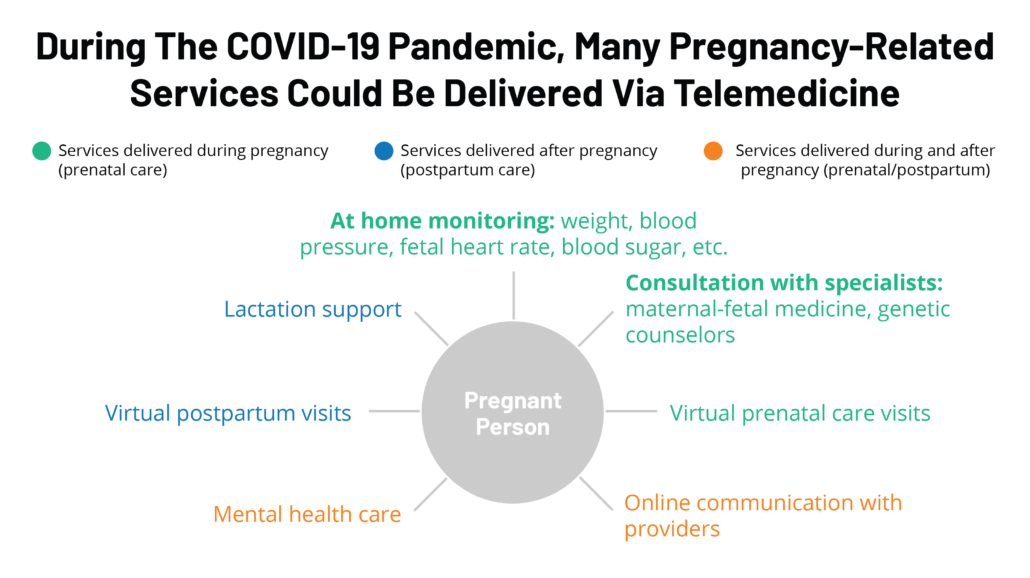
- medical problems, such as depression, sleep apnea, or chronic pain
- caring for another person during the night
Health issues that commonly disrupt sleep include:
- chronic fatigue syndrome
- chronic pain
- substance misuse
- depression
- anxiety
- bipolar disorder
- schizophrenia
- obesity
- sleep apnea
- bruxism, or grinding the teeth
- narcolepsy