What to know about endometriosis
Endometriosis is an incurable but manageable gynecological condition.
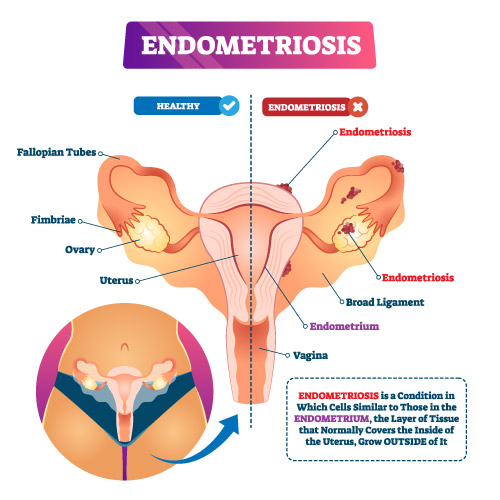
It occurs when endometrial implants, comprised of tissue normally found within the uterus, are present in other areas of the body.
As the tissue continues to thicken, break down, respond to menstrual cycle hormones, and bleed during the menstrual cycle, endometriosis forms deep inside the body.
Scar tissue and adhesions form, and this can cause organ fusion and anatomical changes.
Endometriosis is thought to affect around 11 percent of women in the United States aged between 15 and 44 years.
Fast facts on endometriosis
Here are some key points about endometriosis. More information is in the main article.
- Endometriosis affects between 6 and 10 percent of women of reproductive age worldwide.
- The condition appears to be present in a developing fetus, but estrogen levels during puberty are thought to trigger the symptoms.
- Symptoms are generally present during the reproductive years.
- Most women go undiagnosed, and in the U.S. it can take around 10 years to receive a diagnosis.
- Allergies, asthma, chemical sensitivities, autoimmune diseases, chronic fatigue syndrome, fibromyalgia, breast cancer, and ovarian cancer are linked to women and families with endometriosis.
What is endometriosis?
Endometrial tissue consists of gland, blood cells, and connective tissue. It normally grows in the uterus, to prepare the lining of the womb for ovulation.
Endometrial implants are buildups of endometrial tissue that grow in locations outside the uterus.
When they grow outside the uterus, this is called endometriosis.
They can develop anywhere in the body, but they usually occur in the pelvic area.
They may affect:
- the ovaries
- the fallopian tubes
- the peritoneum
- the lymph nodes
Normally, this tissue is expelled during menstruation, but displaced tissue cannot do this.
This leads to physical symptoms, such as pain. As the lesions grow larger, they can affect bodily functions. For example, the fallopian tubes may be blocked.
The pain and other symptoms can affect different areas of life, including the ability to work, medical care costs, and difficulty maintaining relationships.
Symptoms
Other medical conditions such as pelvic inflammatory disease (PID), ovarian cysts, and irritable bowel syndrome (IBS) can mimic the symptoms of endometriosis.
Symptoms of endometriosis include:
- Severe menstrual cramps, unrelieved with NSAIDS
- Long-term lower-back and pelvic pain
- Periods lasting longer than 7 days
- Heavy menstrual bleeding where the pad or tampon needs changing every 1 to 2 hours
- Bowel and urinary problems including pain, diarrhea, constipation, and bloating
- Bloody stool or urine
- Nausea and vomiting
- Fatigue
- Pain during intercourse
- Spotting or bleeding between periods
Pain is the most common indication of endometriosis, but the severity of the pain does not always correlate with the extent of the disease.
Pain often resolves following menopause, when the body stops producing estrogen production. However, if hormone therapy is used during menopause, symptoms may persist.
Pregnancy may provide temporary relief from symptoms.
Complications
Complications include:
- infertility, which can affect 50 percent of those with the condition.
- increased risk of developing ovarian cancer or endometriosis-associated adenocarcinoma
- ovarian cysts
- inflammation
- scar tissue and adhesion development
- intestinal and bladder complications
It is important to see a health care provider about symptoms, to avoid future complications.
Treatment
Surgery is possible, but it is normally considered only if other treatments are not effective.
Other options include:
Pain medications: Either over-the-counter (OTC) nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB, others) or prescription drugs for the treatment of painful menses.
Hormones: Treatment may be with hormonal therapies such as hormonal birth control, Gonadotropin-releasing hormone (Gn-RH) agonists and antagonists, Medroxyprogesterone (Depo-Provera) or Danazol. Placement of an intrauterine device (IUD) may also be recommended.
Surgery: Initial surgery will seek to remove the areas of endometriosis, but a hysterectomy with removal of both ovaries may be necessary.
Fertility treatment: Pregnancy may be recommended via in-vitro fertilization (IVF).
Managing symptoms at home
Complementary and alternative treatments may include acupuncture, chiropractic, and herbal medicine, but there is little evidence to show that these are effective.
Avoiding caffeine may help to reduce pain, as caffeine can worsen symptoms.
Exercise, such as walking, may reduce pain and slow the progress of the condition by reducing estrogen levels.
It is important to monitor symptoms, because of the long-term complications of endometriosis. Intolerable pain or unexpected bleeding should be reported to a doctor.
Although there is currently no cure for endometriosis, most women are able to relieve the pain of symptoms and will still be able to have children.
Diagnosis
Diagnosis can be challenging because there is no single test for evaluation.
The only way to truly confirm the condition is by undergoing a surgical laparoscopy.
A surgical laparoscopy is a minimally invasive procedure in which a thin, lighted tube with a miniature camera attached, called a laparoscope, is inserted through a small incision in the pelvic area.
A diagnosis can be categorized as follows:
- Stage 1: Lesions are minimal and isolated
- Stage 2: Lesions are mild. There may be several and adhesions are possible.
- Stage 3: Lesions are moderate, deep or superficial with clear adhesions
- Stage 4: Lesions are multiple and severe, both superficial and deep, with prominent adhesions.
It can take many years to receive a diagnosis.
Other possible diagnostic strategies include a pelvic exam, radiologic imaging with ultrasound or magnetic resonance imaging (MRI), and the use of certain medications including birth control or gonadotropin releasing hormone (GnRH) agonists.
Diet
Dietary steps have been suggested for managing the pain and effects of endometriosis.
A 2004 study suggests that a brown seaweed called bladderwrack may have an estrogen-reducing effect in women. This can reduce the growth rate of endometriosis.
One author presented a case study using a diet low in short-chain-fermentable carbohydrates to reduce the symptoms of endometriosis. This diet has been shown to work on IBS and since it is often found with endometriosis, then perhaps the diet would be effective for those with only endometriosis.
More research is needed, but there is little harm in trying this approach.
Dietary choices have also been linked to the development of endometriosis. A study carried out in 2011 suggested that fruit intake increased the risk of endometriosis and a higher total fat intake decreased the risk.
Dairy products were also shown to reduce the risk of endometriosis, although these results were not statistically significant.
Eating yogurt, sauerkraut, and pickles or finding a good source of probiotics may help reduce gastrointestinal symptoms and cause increased digestive activity.
Avoiding caffeine may help to reduce pain, as caffeine can worsen symptoms.

Leave a Reply
Want to join the discussion?Feel free to contribute!