What to know about COVID-19 symptoms in children
Although there are notable exceptions, most evidence suggests that COVID-19 is much less dangerous for children than it is for adults and infants.
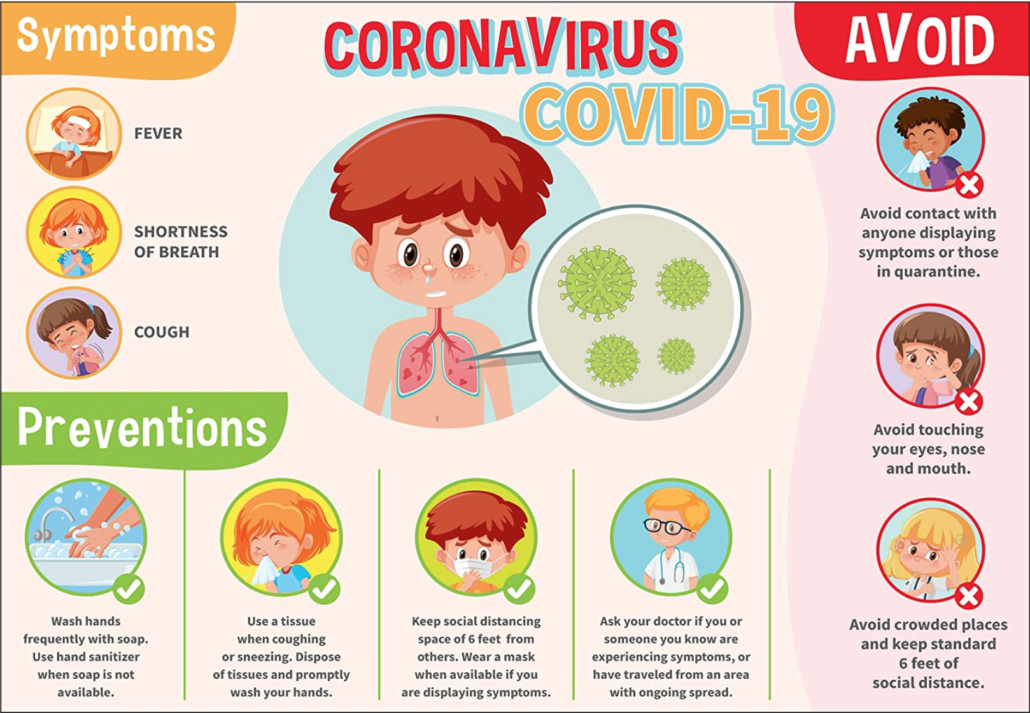
Knowing the symptoms of COVID-19 in children can help parents and caregivers identify the emergency warning signs and seek appropriate care.
This article covers the symptoms of COVID-19 in children, some potential complications, and when to see a doctor.
Symptoms of COVID-19 in children
Data from both China and the United States on children with SARS-CoV-2, the virus that causes COVID-19, suggest that the risk of severe illness is lower in children than it is in adults.
A study of 2,752 cases of COVID-19 in children found that three had died, though the exact cause of death in each case is under investigation.
Current evidence suggests that infants have a higher rate of hospitalization, with some requiring treatment in intensive care units.
In China, more than 90% of children with COVID-19 had no symptoms and only mild-to-moderate disease.
The following are some symptoms that children may experience:
- Fever: Although most adults report a fever with COVID-19, fevers are slightly less common among children, according to data from the Centers for Disease Control and Prevention (CDC).
- Flu-like symptoms: Around 73% of children with COVID-19 had a fever, cough, or shortness of breath. Shortness of breath is much less common in children. In one analysis, 43% of adults and just 13% of children had this symptom.
- Respiratory tract symptoms: Children with mild forms of the illness may develop a runny nose, cough, or sore throat.
- Digestive symptoms: Some children develop vomiting, diarrhea, or nausea.
- Changes in the sense of smell: A 2020 analysis found that most adults with COVID-19 lose their sense of smell. Researchers have not assessed this symptom in young people, but children may also lose their sense of taste or smell.
- Pain: Children with COVID-19 may develop muscle pain or a headache.
- Behavioral changes: Children may be moody or cry more often, especially if they are too young to verbally express their emotions or identify their symptoms. Some children may also be anxious, especially if they know that COVID-19 can be dangerous.
Overall, COVID-19 symptoms tend to be less severe in children. Children are also less likely than adults to report each symptom.
Complications
Children with underlying health conditions — such as lung disease, heart disease, or a weak immune system — are more susceptible to serious COVID-19 complications.
A CDC study that assessed COVID-19 symptoms in children used data on hospitalization and underlying medical conditions for 295 children. In that group, 77% of hospitalized children had at least one other medical condition. This suggests that comorbidities are a significant risk factor for hospitalization in children.
Even among high risk children, however, the risk of dying from COVID-19 is very low. Of 2,143 children included in a Chinese CDC study, just one 14-year-old died. Also, as above, 3 out of 2,572 children in a CDC study died, though the cause in each case is currently unconfirmed.
Some other potential complications include:
- organ failure
- the need to use a ventilator
- sepsis, which is a severe infection that affects many systems in the body
- heart failure
- issues that can cause life threatening blood clots
Children with severe symptoms usually develop them within a week of getting sick.
A small number of children have also developed symptoms of multisystem inflammatory syndrome in children (MIS-C). This syndrome can cause symptoms that resemble those of toxic shock syndrome and Kawasaki disease. Without treatment, it may be fatal.
Children with MIS-C may develop a rash, stomach pain, bloodshot eyes, exhaustion, diarrhea, or vomiting.
The following symptoms require emergency medical attention:
- confusion
- fever
- chest pressure or pain
- neck pain
- difficulty breathing
- blue or white face, fingers, or toes
- an inability to stay awake
- severe stomach pain
When to see a doctor
Most children have either no symptoms or only mild-to-moderate ones. These children do not need to go to the hospital or see a doctor.
However, parents and caregivers should call a pediatrician if their child shows any symptoms of COVID-19. The pediatrician can offer advice on which symptoms to watch and some suggestions for home treatment.
In some areas, a child may also need a referral for COVID-19 testing.
Call a doctor if:
- the child seems very ill
- they develop a rash
- their symptoms get better and then get worse again
- they recover from COVID-19 but then develop inflammatory symptoms, such as a rash, fever, or bloodshot eyes
Go to the emergency room if a child:
- gasps for air or shows signs of respiratory distress, such as bluish lips, breathing very fast, or difficulty breathing
- seems confused, seems lethargic, or cannot wake up
- reports pressure or pain in their chest
- has symptoms of organ failure, such as intense pain in the stomach, difficulty passing urine, an inability to move without help, or an inability to think clearly
Treatment
No medication can cure COVID-19. Although hospitals and researchers are exploring experimental treatments, these are currently only available to very sick people.
Most children can recover with home treatment. To help a child with COVID-19:
- Encourage them to rest.
- Give them lots of fluids to prevent dehydration.
- Check on them regularly to ensure that they are not getting worse.
- Ask a doctor about over-the-counter pain and fever relievers.
- Have them stay in a single area of the house, if possible. Clean and disinfect all surfaces they touch, and encourage other family members to avoid them. Also, wear a face mask when caring for a sick child.
Parents and caregivers may find these guidelines challenging to follow when caring for a child or infant. The CDC offer some advice on how to manage risk around children.
It may also be a good idea to speak to a medical professional about how best to care for a child with a suspected SARS-CoV-2 infection. Children under 2 years of age should not wear a face covering.
Very sick children may need to go to the hospital. In the hospital, doctors will focus on managing the child’s symptoms. They might need oxygen, intravenous fluids, or steroid medications to help them breathe.
Rarely, a child might need a ventilator if they cannot breathe well on their own.

Leave a Reply
Want to join the discussion?Feel free to contribute!