Depression is a mental health condition that causes a chronic feeling of emptiness, sadness, or inability to feel pleasure that may appear to happen for no clear reason.
Depression is the leading cause of disability worldwide, according to the World Health Organization (WHO).
It can undermine a person’s relationships, make working and maintaining good health very difficult, and in severe cases, may lead to suicide. In fact, depression contributes to nearly 40,000 suicides in the United States each year.
It can affect adults, adolescents, and children. This article examines what depression is and what causes it, as well as types of depression, treatment, and more.
Depression is a mood disorder that causes persistent feelings of sadness, emptiness, and loss of joy. It is different from the mood fluctuations that people regularly experience as a part of life.
Major life events, such as bereavement or the loss of a job, can trigger depression. But depression is distinct from the negative feelings a person may temporarily have in response to a difficult life event.
Depression often persists in spite of a change of circumstances and causes feelings that are intense, chronic, and not proportional to a person’s circumstances.
It is an ongoing problem, not a passing one. While there are different types of depression, the most common one is major depressive disorder. It consists of episodes during which the symptoms last for at least two weeks.
Depression can last for several weeks, months, or years. For many people, it is a chronic illness that gets better and then relapses.
While there is no cure for depression, there are effective treatments that help with recovery. The earlier that treatment starts, the more successful it may be. Some people may never experience depression again after a single period of it. Others will continue to have relapses.
Many people experiencing depression recover after a treatment plan. Even with effective treatment, however, a relapse may occur. About half of people do not initially respond to treatment.
To prevent relapse, people who take medication for depression should continue with treatment — even after symptoms improve or go away — for as long as their doctor advises.
Find tips to help prevent depression from returning here.
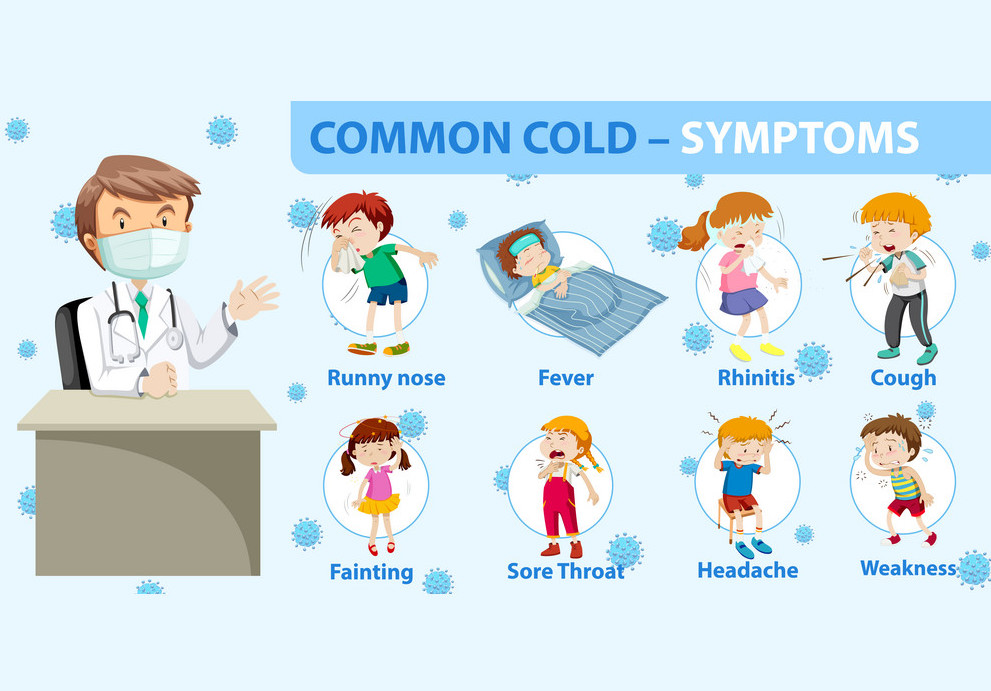
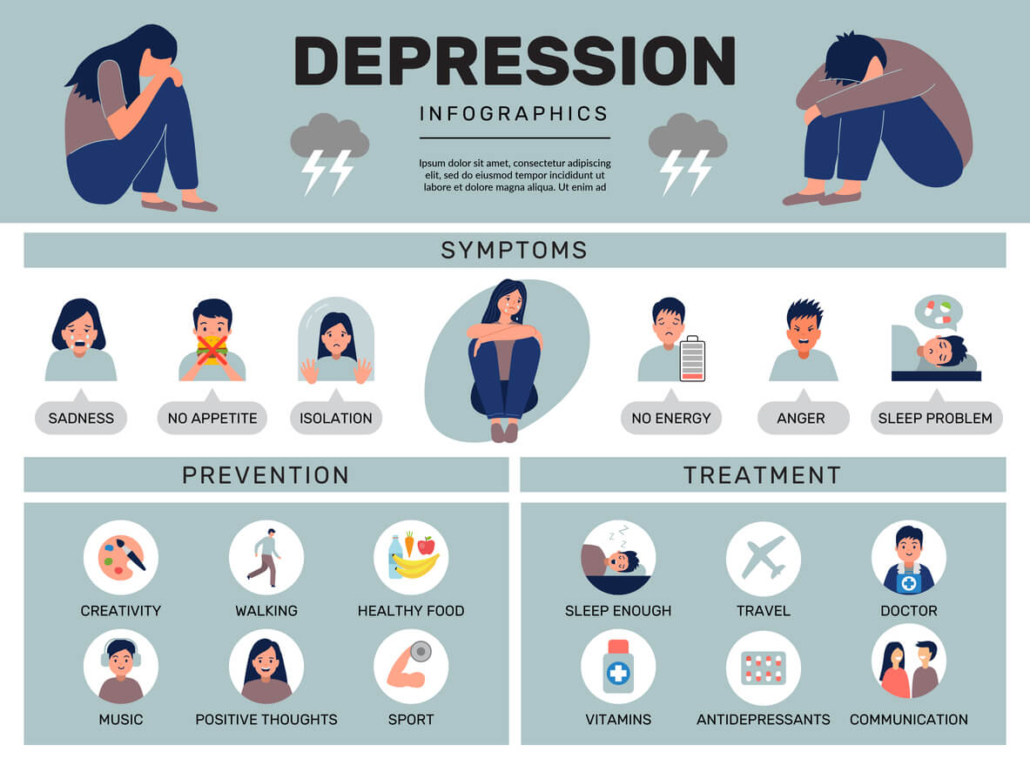
Depression can cause a range of psychological and physical symptoms, including
- persistent depressed mood
- loss of interest or pleasure in hobbies and activities
- changes in appetite and body weight
- unusually slow or agitated movements
- decreased energy or fatigue
- difficulty sleeping or oversleeping
- excessive feelings of guilt or worthlessness
- difficulty concentrating or making decisions
- thoughts of death or suicide, or suicide attempts
If a person experiences five Trusted Sourceor more of these symptoms during the same 2-week period, a doctor may diagnose them with depression.
Depression may also cause other symptoms, including irritability, restlessness, chronic pain, headaches, and digestive issues.
There are several forms of depression. Below are some of the most common types.
Major depression
A person living with major depression experiences a constant state of sadness. They may lose interest in activities they used to enjoy.
Treatment usually involves medication and psychotherapy.
Persistent depressive disorder
Also known as dysthymia, persistent depressive disorder causes symptoms that last for at least 2 years.
A person living with this disorder may have episodes of major depression as well as milder symptoms that do not meet the criteria for major depressive disorder.
Postpartum depression
After giving birth, some people experience a brief period of sadness or heightened emotions that some people call the “baby blues.” This usually goes away in a few days to a few weeks.
Postpartum depression, or postnatal depression, is more severe.
There is no single cause for this type of depression, and it can persist for months or years. Anyone who experiences ongoing depression after delivery should seek medical attention.
Major depressive disorder with seasonal pattern
Previously known as seasonal affective disorder (SAD), this type of depression usually occurs during the winter and fall months, when there is less daylight. Less commonly, it may follow other seasonal patterns.
It lifts during the rest of the year and in response to light therapy.
This condition seems to particularly affect people who live in countries with long or severe winters.
The medical community does not fully understand the causes of depression. There are many possible causes, and sometimes, various factors combine to trigger symptoms.
Factors that are likely to play a role include:
- genetic features
- changes in the brain’s neurotransmitter levels
- environmental factors such as exposure to trauma or lack of social support
- psychological and social factors
- additional conditions, such as bipolar disorder
Interactions between various factors can increase the risk of depression. For instance, a person with a family history or a genetic risk of depression may experience symptoms of depression following a traumatic event.
The symptoms of depression can include:
- a depressed mood
- reduced interest or pleasure in activities that a person previously enjoyed
- a loss of sexual desire
- changes in appetite
- unintentional weight loss or gain
- sleeping too much or too little
- agitation, restlessness, and pacing up and down
- slowed movement and speech
- fatigue or loss of energy
- feelings of worthlessness or guilt
- difficulty thinking, concentrating, or making decisions
- recurrent thoughts of death or suicide, or an attempt at suicide
Find out more about recognizing the hidden signs of depression here.
In females
Depression is nearly twice as common in females than males, according to the Centers for Disease Control and Prevention (CDC).
Researchers do not know why depression appears to be more common in females. However, a 2021 study proposes that the difference may be due to disparities in reporting. Researchers found that females were more likely than males to report and seek treatment for depression symptoms.
Some research suggests that exposure to gender discrimination increases the risk of depression.
Also, some types of depression are unique to females, such as postpartum depression and premenstrual dysphoric disorder.
In males
According to data from the National Health and Nutrition study, which relies on self-reports of mental health symptoms, 5.5% of males report depression symptoms in a given 2-week period, compared with 10.4% of females.
Males with depression are more likely than females to drink alcohol in excess, display anger, and engage in risk-taking as a result of the disorder.
Other symptoms of depression in males may include:
- avoiding family and social situations
- working without a break
- having difficulty keeping up with work and family responsibilities
- displaying abusive or controlling behavior in relationships
Learn more about the symptoms of depression in men.
In college students
Time at college can be stressful, and a person may be dealing with other lifestyles, cultures, and experiences for the first time.
Some students have difficulty coping with these changes, and they may develop depression, anxiety, or both as a result.
Symptoms of depression in college students may include:
- difficulty concentrating on schoolwork
- insomnia
- sleeping too much
- a decrease or increase in appetite
- avoiding social situations and activities that they used to enjoy
In teens
Physical changes, peer pressure, and other factors can contribute to depression in teenagers.
They may experience some of the following symptoms:
- feeling irritable
- restlessness, such as an inability to sit still
- withdrawing from friends and family
- difficulty concentrating on schoolwork
- feeling guilty, helpless, or worthless
In children
The CDC estimate that, in the U.S., 4.4% of children and teenagers aged 3–17 have a diagnosis of depression. This figure has risen in recent years.
Depression in children can make schoolwork and social activities challenging. They may experience symptoms such as:
- crying
- low energy
- clinginess
- defiant behavior
- vocal outbursts
Younger children may have difficulty expressing how they feel in words. This can make it harder for them to explain their feelings of sadness.
Learn more about mental health in trans people here.
In historically marginalized groups
Research shows that the prevalence of major depression among African Americans has been around 10.4%, compared with 17.9% among people who are white.
However, 56% of African Americans experience depression more chronically, compared with 38.6% of people who are white. This implies that though fewer African Americans may experience depression, those who do may experience it for longer. In addition, less than half of these African Americans have sought treatment.
Other research indicates that African Americans may have depression less frequently than non-Hispanic people who are white, but this may be due to the fact that many African Americans often do not have a proper diagnosis.
Triggers are emotional, psychological, or physical events or circumstances that can cause depression symptoms to appear or return.
These are some of the most common triggers:
- stressful life events, such as loss, family conflicts, and changes in relationships
- incomplete recovery after having stopped depression treatment too soon
- medical conditions, especially a medical crisis such as a new diagnosis or a chronic illness such as heart disease or diabetes
Find out more about depression triggers here.
Some people have a higher risk of depression than others.
Risk factors include:
- experiencing certain life events, such as bereavement, work issues, changes in relationships, financial problems, and medical concerns
- experiencing acute stress
- having a lack of successful coping strategies
- having a close relative with depression
- using some prescription drugs, such as corticosteroids, certain beta-blockers, and interferon
- using recreational drugs, such as alcohol or amphetamines
- having sustained a head injury
- having a neurodegenerative disease such as Alzheimer’s or Parkinson’s
- having had a previous episode of major depression
- having a chronic condition, such as diabetes, chronic obstructive pulmonary disease (COPD), or cardiovascular disease
- living with chronic pain
- lacking social support
Depression can also occur as a symptom or comorbidity with another mental health condition. Examples include:
Psychotic depression
Psychosis can involve delusions, such as false beliefs and a detachment from reality. It can also involve hallucinations — sensing things that do not exist.
Some people experience depression with psychosis. A person living with psychosis, which is a serious psychiatric illness, may experience depression as a result.
Alternatively, a person living with depression may have a severe form of the condition that also includes psychosis symptoms.
Bipolar disorder
Depression is a common symptom of bipolar disorder. People with bipolar disorder experience periods of depression that may last weeks. They also experience periods of mania, which is an elevated mood that may cause a person to feel very happy, aggressive, or out of control.
What does bipolar disorder involve, and what types are there? Find out here.
Depression is treatable, though the treatment may depend on the exact type a person is living with.
However, about 30.9% of people do not respond to treatment or respond poorly. About 4 in 10 people achieve remission of their symptoms within 12 months, but depression can come back.
Managing symptoms usually involves three components:
- Support: This can range from discussing practical solutions and possible causes to educating family members.
- Psychotherapy: Also known as talking therapy, some options include one-to-one counseling and cognitive behavioral therapy (CBT).
- Drug treatment: A doctor may prescribe antidepressants.
Medication
Antidepressants can help treat moderate to severe depression. Several classes of antidepressants are available:
- selective serotonin reuptake inhibitors (SSRIs)
- selective serotonin and norepinephrine reuptake inhibitors (SNRIs)
- atypical antidepressants
- tricyclic antidepressants
- monoamine oxidase inhibitors (MAOIs)
Each class acts on a different neurotransmitter or combination of neurotransmitters.
A person should only take these medications as their doctor prescribes. Some drugs can take a while to have an impact. By stopping taking the drug, a person may not experience the benefits that it can offer.
Some people stop taking medication after symptoms improve, but this can lead to a relapse.
A person should raise any concerns about antidepressants with a doctor, including any intention to stop taking the medication.
Learn more about antidepressants and how they can help here.
Medication side effects
SSRIs and SNRIs can have side effects. A person may experience:
- nausea
- constipation
- diarrhea
- low blood sugar
- weight loss or weight gain
- a rash
- sexual dysfunction
Find out more about the possible side effects of antidepressants here.
The Food and Drug Administration (FDA) requires manufacturers to put a “black box” warning on antidepressant bottles.
The warning indicates that, among other risks, these medications may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment. While there is an increase in risk, the absolute risk remains low.
Natural remedies
Some people use natural remedies, such as herbal medicines, to treat mild to moderate depression.
However, since the FDA does not monitor herbal remedies, manufacturers may not be truthful about the quality of these products. They may not be safe or effective.
In a 2018 systematic review of herbal remedies for depression, 45% of studies reported positive results from herbal treatments, including fewer side effects than standard antidepressants.
The following are some of the more popular herbs and plants that people use to treat depression:
- St. John’s wort: This is not suitable for people who are or may be living with bipolar disorder. Learn more here.
- Ginseng: Practitioners of traditional medication may use this to improve mental clarity and reduce stress. Find out more about ginseng here.
- Chamomile: This contains flavonoids that can have an antidepressant effect. For more information about chamomile, click here.
- Lavender: This may help reduce anxiety and insomnia. Learn more about lavender here.
It is essential for a person to speak with a doctor before using any type of herbal remedy or supplement to treat depression. Some herbs can interfere with the action of drugs or otherwise make symptoms worse.
Supplements
A person may take the herbs above as supplements to treat symptoms of mild to moderate depression. Other types of supplements can also help treat these symptoms.
It is important to remember that the FDA does not monitor supplements to ensure that they are effective or safe.
Nonherbal supplements that may help treat depression include S-adenosyl methionine (SAMe) — a synthetic form of a natural chemical in the body. They also include 5-hydroxytryptophan, which can help to boost serotonin, the neurotransmitter in the brain that affects a person’s mood.
Some research has suggested that SAMe may be as helpful as the prescription antidepressants imipramine and escitalopram, but more investigation is necessary.
Learn more about how herbs and supplements may help relieve depression here.
Food and diet
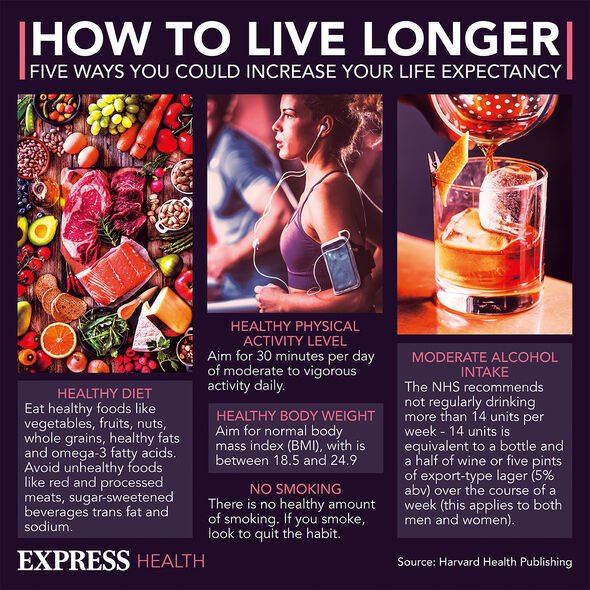
Some research suggests that eating a lot of sugary or processed foods can lead to various physical health problems and poor mental health. Results of a 2019 study suggest that a diet that includes many of these types of food can affect the mental health of young adults.
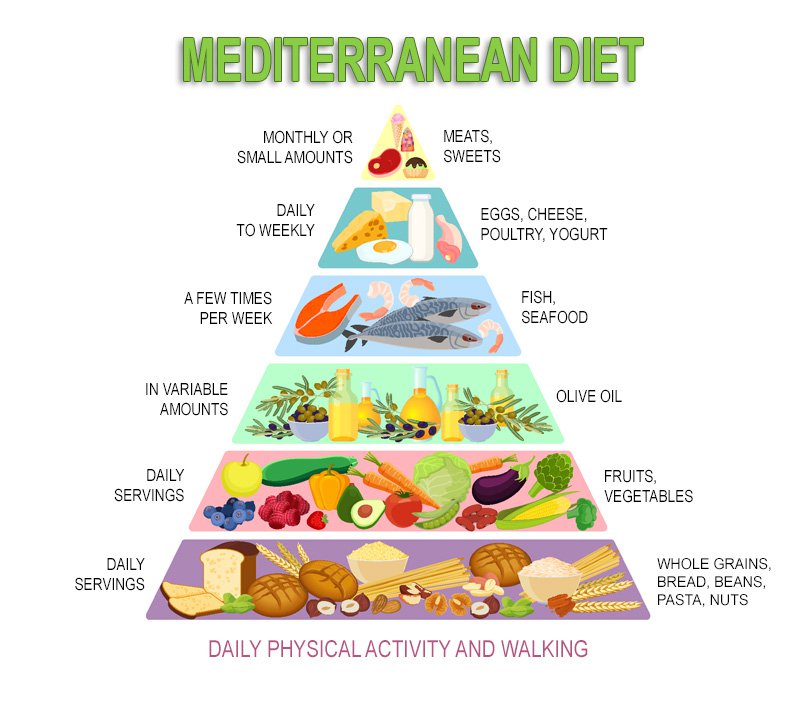
The study also found that eating more of the following foods helped reduce depression symptoms:
- fruit
- vegetables
- fish
- olive oil
Can other foods worsen or improve depression symptoms? Find out here.
Psychotherapy
Psychotherapy, or talking therapies, for depression include CBT, interpersonal psychotherapy, and problem-solving treatment.
For some forms of depression, psychotherapy is usually the first-line treatment, while some people respond better to a combination of psychotherapy and medications.
CBT and interpersonal psychotherapy are the two main types of psychotherapy for depression. A person may have CBT in individual sessions with a therapist, in groups, over the telephone, or online.
CBT focuses on helping a person identify the connection between their thoughts, behaviors, and feelings. They then work steadily to change harmful thoughts and behaviors.
Interpersonal therapy aims to help people identify:
- emotional problems that affect relationships and communication
- how these issues also affect their mood
- how to improve relationships and better manage emotions
Exercise
Aerobic exercise raises endorphin levels and stimulates neurotransmitters, potentially easing depression and anxiety. A 2019 paper states that exercise may be especially helpful with treatment-resistant depression.
Exercise offers the greatest benefits when a person combines it with standard treatments, such as antidepressants and psychotherapy.
Brain stimulation therapies
Brain stimulation therapies are another treatment option. For example, repetitive transcranial magnetic stimulation sends magnetic pulses to the brain, and this may help treat major depression.
If depression does not respond to drug treatment, a person may benefit from electroconvulsive therapy (ECT). Doctors do not fully understand how ECT works.
During the procedure, a person is asleep, and a doctor uses electricity to induce a seizure. This may help “reset” the brain, correcting problems with neurotransmitters or other issues that cause depression.
If a person suspects that they have symptoms of depression, they should seek professional help from a doctor or mental health specialist.
A qualified health professional can rule out various causes, ensure an accurate diagnosis, and provide safe and effective treatment.
They will ask questions about symptoms, such as how long they have been present. A doctor may also conduct an examination to check for physical causes and order a blood test to rule out other health conditions.
What is the difference between situational and clinical depression? Find out here.
Tests
Mental health professionals often ask people to complete questionnaires to help assess the severity of their depression.
The Hamilton Depression Rating Scale, for example, has 21 questions. The scores indicate the severity of depression among people who already have a diagnosis.
The Beck Depression Inventory is another questionnaire that helps mental health professionals measure a person’s symptoms.
National hotlines provide free, confidential assistance from trained professionals 24 hours a day. They may benefit anyone with depression who wants or needs to talk about their feelings.
Some of the support hotlines available include:
- Samaritans: This nonprofit organization offers emotional support to anyone who has feelings of depression or loneliness or who is considering suicide. Call or text 877-870-4673 (HOPE).
- National Suicide Prevention Lifeline: Call 1-800-273- 8255 (TALK) to speak with someone from this national network of local crisis centers.
- Lifeline Chat: This is an online chat service of the National Suicide Prevention Lifeline.
- Postpartum Support International: Call 1-800-944-4773. This organization helps people struggling with postpartum depression, as well as other mental health issues that are related to pregnancy, birth, and new parenthood.
A person with a parent or sibling who has depression is about three times more likely than other people to develop the condition.
However, many people with depression have no family history of it.
A recent study suggests that susceptibility to depression may not result from genetic variation. The researchers acknowledge that while people can inherit depression, many other issues also influence its development.
Learn more about whether depression has a genetic link here.
Depression is the leading cause of disability around the world, according to the WHO.
In the U.S., the Social Security Administration considers depressive, bipolar, and related disorders to be disabilities. If a person’s depression prevents them from working, they may qualify for social security disability insurance benefits.
The person must have worked long enough and recently enough to qualify for disability benefits. For more information, visit the administration’s website.
According to the CDC, about 11% of physician office visits note depression on the medical record. The figure is similar for emergency department visits.
Also according to the CDC, 4.4% of children and adolescents between the ages of 3 and 17 years — about 2.7 million people in the U.S. — have a diagnosis of depression.
The CDC also note that 4.7% of American adults have regular feelings of depression.
Here are some common questions about depression.
What does depression do to the brain?
Depression can lead to changes in levels of neurotransmitters, which are molecules that transmit messages between nerve cells. In the long run, it may also cause physical changes to the brain, including reductions in grey matter volume and increased inflammation.
Does depression change your personality?
Research has turned up mixed results about whether or not depression can actually change a person’s personality.
However, according to one review of 10 studies, depressive symptoms may be associated with changes in several specific aspects of personality — including extraversion, neuroticism, and agreeableness — which could be temporary or persistent.
Does depression affect your thinking?
Depression can alter concentration and decision-making. It may also impair attention and cause issues with information processing and memory.
Depression is a serious, chronic medical condition that can affect every aspect of a person’s life. When it causes suicidal thoughts, it can be fatal.
People cannot think their way out of depression. Depression is not a personal failing or a sign of weakness. It is treatable, and seeking treatment early may increase the chances of recovery.
Because depression can be challenging to treat, it is important for a person to see a doctor with expertise in depression and to be willing to try several different treatments. Often, a combination of therapy and medication offers the best results.